Thank you, Jess, for sharing your story with us. She points out right away that all babies are miracles. I completely agree with that and would add that babies are also resilient. I think it is a great testimony to the resiliency of babies, and human life, that despite such a risky situation little Juliette was born in such great health!
NICUdiaries is place that celebrates the progress made by babies who have had a rough start to life.
Anyone is welcome to share their story here.
If you have a story you'd like to share feel free to email me annagcoyne@gmail.com
If you have a story you'd like to share feel free to email me annagcoyne@gmail.com
The views expressed are those of the guest writers
and do not necessarily reflect of the views of k n i t o n e y a r n o v e r.
Juliet
came into the world like a firecracker, despite everyone's best efforts to stop
her. I feel like our NICU journey starts
at the moment we found out I was pregnant, although we would have never
imagined this would be our story.
She is literally a miracle from conception (as all babies are). My first pregnancy had been a breeze. I felt amazing and had none of the normal pregnancy induced side effects like morning sickness. In December 2012 after an easy labor and delivery I gave birth to a 41 week, 8lb 3oz clone of my husband, Jaslyn Jean. We were smitten. Since I was exclusively breast feeding, I chose to use a Paragaurd IUD as birth control. My plan was to leave it in until Jaslyn was about 18 months old and then we would try for baby #2.
Fast forward to October 2013. Jaslyn was 10 months old and I was working full time and finishing my doctorate in nursing. I was unnaturally tired and just generally felt poorly, but I had a new baby and crazy stress and responsibilities, so I wasn't concerned. My mom kept telling me I needed to take a pregnancy test, but I kept reassuring her the Paragaurd was one of the most effective forms of birth control and there was no way I was pregnant. Plus, I was still exclusively nursing Jaslyn and we had to use some fertility medication to even conceive her -- there was no way I had randomly gotten pregnant with all of those things working against a baby.
My mom finally convinces me to take a test, which is positive, but a pregnancy is impossible because I have this very very effective form of birth control. I go to my OB, who also thinks the test was likely a false positive or maybe I have a tubal pregnancy. We immediately go for an ultrasound which reveals....
One healthy, viable, 10 week old fetus. Say what?!?!
Since my doctor had never had this happen to a patient, we did not really know what to expect. I went to WVU to see a high risk perinatologist, who tried to remove the IUD but was unsuccessful. Somewhere in the course of 3-4 days the IUD had moved from my cervix to the top of my uterus, above the baby. And there it remained for the remainder of the pregnancy.
My pregnancy progressed mostly as normal with no major compilations through 7 months. There was a risk that the IUD would move closer to the cervix as the pregnancy progressed and that premature labor might be a risk. There were lots of women, however, who had delivered fullterm babies with an IUD. I felt terrible though. Constantly tired. Horrible hip and back pain. Nausea and vomiting. Nothing like my first babe. The Sunday of my 30th week, I started having contractions. Over the next few days I made multiple trips to the labor and delivery unit but was always sent home and advised to continue bedrest. On Wednesday, my third trip to L&D ended with my water breaking and me being transferred by ambulance 2.5 hours from home to a large hospital with a NICU. From Wednesday to Saturday the doctors worked to keep my baby from being born. On Saturday morning, they could do no more, and after a wild unmedicated labor, Juliet Todd Wooten made her way into this mad, mad, world.
She is literally a miracle from conception (as all babies are). My first pregnancy had been a breeze. I felt amazing and had none of the normal pregnancy induced side effects like morning sickness. In December 2012 after an easy labor and delivery I gave birth to a 41 week, 8lb 3oz clone of my husband, Jaslyn Jean. We were smitten. Since I was exclusively breast feeding, I chose to use a Paragaurd IUD as birth control. My plan was to leave it in until Jaslyn was about 18 months old and then we would try for baby #2.
Fast forward to October 2013. Jaslyn was 10 months old and I was working full time and finishing my doctorate in nursing. I was unnaturally tired and just generally felt poorly, but I had a new baby and crazy stress and responsibilities, so I wasn't concerned. My mom kept telling me I needed to take a pregnancy test, but I kept reassuring her the Paragaurd was one of the most effective forms of birth control and there was no way I was pregnant. Plus, I was still exclusively nursing Jaslyn and we had to use some fertility medication to even conceive her -- there was no way I had randomly gotten pregnant with all of those things working against a baby.
My mom finally convinces me to take a test, which is positive, but a pregnancy is impossible because I have this very very effective form of birth control. I go to my OB, who also thinks the test was likely a false positive or maybe I have a tubal pregnancy. We immediately go for an ultrasound which reveals....
One healthy, viable, 10 week old fetus. Say what?!?!
Since my doctor had never had this happen to a patient, we did not really know what to expect. I went to WVU to see a high risk perinatologist, who tried to remove the IUD but was unsuccessful. Somewhere in the course of 3-4 days the IUD had moved from my cervix to the top of my uterus, above the baby. And there it remained for the remainder of the pregnancy.
My pregnancy progressed mostly as normal with no major compilations through 7 months. There was a risk that the IUD would move closer to the cervix as the pregnancy progressed and that premature labor might be a risk. There were lots of women, however, who had delivered fullterm babies with an IUD. I felt terrible though. Constantly tired. Horrible hip and back pain. Nausea and vomiting. Nothing like my first babe. The Sunday of my 30th week, I started having contractions. Over the next few days I made multiple trips to the labor and delivery unit but was always sent home and advised to continue bedrest. On Wednesday, my third trip to L&D ended with my water breaking and me being transferred by ambulance 2.5 hours from home to a large hospital with a NICU. From Wednesday to Saturday the doctors worked to keep my baby from being born. On Saturday morning, they could do no more, and after a wild unmedicated labor, Juliet Todd Wooten made her way into this mad, mad, world.
Juliet
was admitted to the NICU for prematurity alone.
By the grace of God she did not suffer any complications from the
delivery or have any major medical problems.
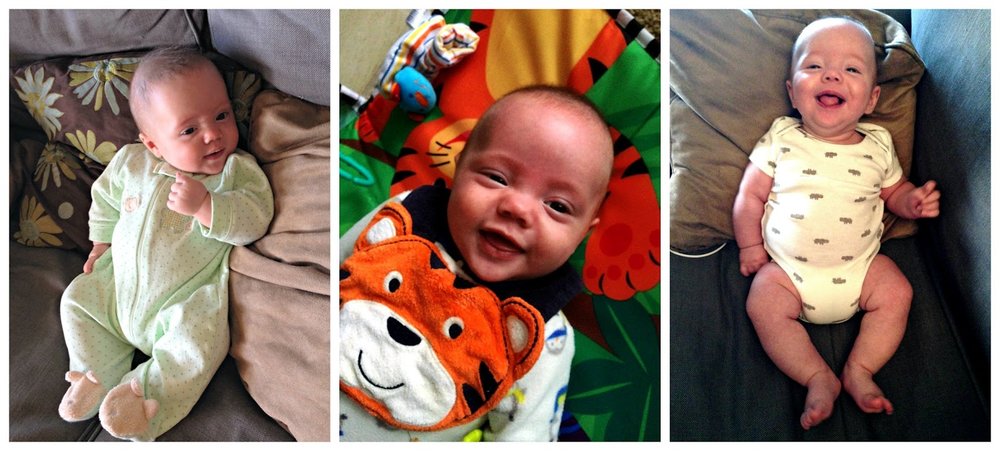
At just 31 weeks, she weighed 4 lbs 1.5oz and required no ventilation or
oxygenation. For the first three days of
her life she received IV fluid and prophylactic antibiotics. She was also under a bili light for jaundice
for days 1-4. My baby was 4 days old
before I ever got to hold her. She sat
in her little incubator with her tiny Ray-Bans and basked in the warmth and
stillness. She did not cry.
I
cried. I cried all day for at least the
first week. I was scared. Even if she was healthy, no one was holding
her, comforting her. What if she was
distressed but the nurses were too busy to go to her. How could I stay by her side and still
continue to take care of my 15 month old at home? I was tired, so tired.
I
feel like the NICU experience is just like a job. You have a baby, and instead of resting,
starting maternity leave, snuggling with your new little one surrounded by all
those you love, you get up and go to work.
You and the baby both. Your baby
works hard to grow. Learns to suck, swallow, and breathe. You wake up the morning after your labor,
pack your breast pump, and head to the office.
You sit there and stare at her, only taking breaks to pump and pee. You leave at night, without the baby that
brought you there, lie sleepless in a strange bed, waking every 3 hours to
pump, and then do it all again the next day.
I struggled with how often I should be at her bedside. The doctors told us we couldn’t be with her
all the time. We needed to take time for
ourselves and our other daughter. I
needed to heal from my crazy birth experience.
But every time I left the nurse said “When are you coming back?” I know they meant nothing by it but I felt so
accountable. So guilty for being outside
the hospital walls while she was within.
And
in the end, we are the lucky ones. The
lucky ones whose baby was strong from the start. We needed no interventions during our stay in
the NICU. No oxygen, no medications. A
single tiny feeding tube in baby’s nose until she could take a bottle. The
doctors were impressed with Juliet’s will.
The nurses called her a firecracker and joked that she thought she was
full-term baby from the start. We stayed
for exactly 3 weeks and took home a 5 lb 8oz baby girl. Having the healthiest baby in the unit makes
you hyper aware of the families around you who aren’t as lucky. But it doesn’t make you feel any better about
your situation. It’s still unnatural.
All wrong. Absolutely
heartbreaking.
We
had amazing care in the NICU and couldn’t be more grateful for the doctors and
nurses who cared for our little love. We had the best in the worst
situation. If I could say anything to the parents who
have yet to go on this journey it would be this: Nothing prepares you for the NICU. No one understands how you feel or what you
are going through except for those parents who have been there before you. Don’t read all the books about preemies, they
will just scare you. Try to sleep. Let others do as much as they can for you
while you focus on your baby. Cry it
out. It isn’t fair and that’s your
right. Get mad. Its natural. Pray. But know that your baby is where they need to
be. The NICU staff will take excellent
care of your baby. Your time there is an eternity and an instant. Take pictures every day because they grow and
change so fast. Before you know it,
you’ll be telling your story…